Cervical Cancer

Screening & Diagnosis Of HPV
Screening Tests: Screening tests for cervical cancer involve taking a sample of cells from the cervix to check for signs of cancer. The Papanicolaou (Pap) test, was for a long time considered the standard method of screening in which cervical samples are checked for the abnormalities in the cervical cells. A sample of cells is collected from the surface of the cervix and vagina with a piece of cotton, a brush, or a small wooden stick and viewed under a microscope for abnormalities. The Pap test has greatly reduced the incidence and mortality due to cervical cancer. More recently, a new test has been introduced, which is more sensitive and is known as the HPV DNA screening test.
Clinical History & Examination: The clinician will ask for the presence of symptoms of cervical cancer (such as abnormal vaginal bleeding, pelvic pain, vaginal discharge, pain or discomfort during sex). A clinical examination will be carried out including looking at the cervix and vagina for abnormalities, an internal pelvic examination to check for lumps or other changes as well as examine the vagina, cervix, uterus, fallopian tubes, ovaries, and rectum.
Colposcopy: If either a screening test is positive or symptoms and signs of cervical cancer are present, a colposcopy is conducted. This test allows the clinician to visualise the cervix in detail, and tissue samples of abnormal areas are taken.
Cone Biopsy: In this type of biopsy, a cone-shaped piece of tissue from the cervix is removed, under anaesthesia. It is examined under a microscope by a pathologist to check for abnormal cancer cells.
Radiological tests: Ultrasound uses high-energy sound waves to form a picture of body tissues and examine the abdominal and pelvic region. Chest x-ray is used to check the lungs and chest for the spread of cervical cancer. Intravenous pyelogram is an x-ray of the urinary tract taken with a special dye to identify any spread of cervical cancer in this region. Computed tomography (CT) scans are used to determine the extent of advancement of the cancer as well as to look for spread of the disease beyond the cervix. Magnetic resonance imaging (MRI) scans are useful due to their accuracy in determining the tumour size and spread of cancer. Positron emission tomography (PET) scan uses a radioactive substance injected into a vein which is particularly useful for detecting the spread of cancer to lymph nodes and other parts of the body.
Treatment Of Cervical Cancer
The management of cervical cancer depends on various factors, including the stage of the cancer, additional health issues, age etc. Surgery, radiation, chemotherapy or a combination may be used.
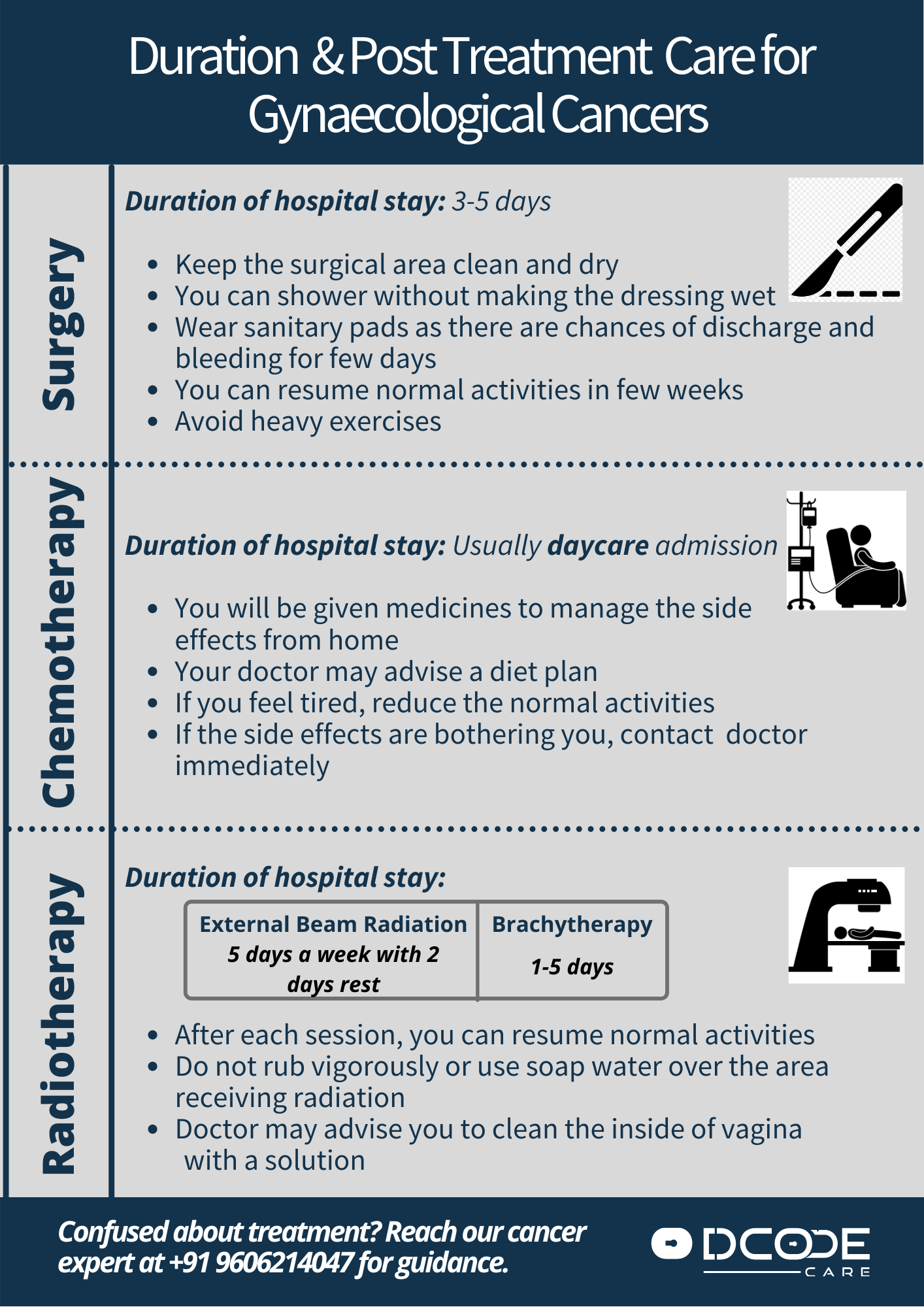
- Surgery: The surgeons aims to remove the tumour as well as a healthy margin of tissue around it. Post-surgery, the tissue is examined under a microscope to ensure complete removal of the tumour. This may involve conisation (removal of a cone-shaped section of the cervix), hysterectomy (uterus and cervix completely removed) or trachelectomy (suitable for very early stage cancer in women who want to have children in the future. The cervix and upper section of the vagina removed, leaving the womb in place). Early-stage cervical cancer is typically treated with surgery to remove the uterus (hysterectomy). A hysterectomy can cure early-stage cervical cancer and prevent recurrence. But removing the uterus also leads to permanent infertility. The types of hysterectomy include Simple hysterectomy (Indicated in very early stage cervical cancer in which only the cervix and uterus are removed along with the tumour), Radical hysterectomy (Cervix, uterus, part of the vagina and lymph nodes are removed). Minimally invasive surgery may be an option for early-stage cervical cancer. Side effects: Side effects depend on the type of surgery but possible adverse effects may include: vaginal bleeding, irregular or painful periods, loss of bladder control, decreased sexual satisfaction, swelling of legs, vaginal prolapse, recurrence of cancer.
- Radiation: This form of therapy uses high-powered energy beams to kill cancer cells. It is used alone or in conjunction with chemotherapy before surgery to reduce the size of the tumour or after surgery to destroy any remaining cancer cells. It is of two types: External beam radiation (the size of radiation is outside the body) or Internal radiation also known as Brachytherapy (a device filled with radioactive material is placed inside the vagina). Side effects: Skin changes, fatigue, skin irritation, bladder inflammation, vaginal bleeding, vaginal dryness, diarrhoea etc.
- Chemotherapy: Chemotherapy uses medications to kill cancer cells. It is often combined with radiation therapy, to enhance the effects of the radiation. In incurable cervical cancers, higher doses of chemotherapy are used to control the disease. Side effects: Adverse effects depend on the drug used as well as the dose. Possible side effects include hair loss, thinning of bones, metallic taste in the mouth, blisters, low immunity, anemia, constipation, fatigue, vomiting, anorexia, joint and muscle pain.
- Targeted Therapy: This form of therapy involves drugs that block specific chemical pathways in cancer cells, thus slowing down or halting growth. Side effects: diarrhoea, vomiting, nausea, fatigue, increased risk of bleeding, low immunity, skin reactions, hypertension, joint pain, nerve damage etc.
- Supportive / Palliative care: Palliative care focuses on providing relief from pain and other symptoms. The main objective is to help cancer patients feel better and live longer and is provided alongside regular clinical care. In patients with advanced cervical cancer, this involves the management of pain, vaginal discharge, fistulae, bleeding, diarrhoea, incontinence, nutrition, and bedsores.
Sources: European Society for Medical Oncology (ESMO); National Cancer Institute; NHS; Mayo Clinic;